A Message on COVID-19 from WorkSTEPS Chief Medical Officer Dr. Ben Hoffman
Take-Aways
- Click-bait reporting on COVID-19, vaccines and vaccinations is going to be a source of distraction, often promoting fear and doubt in months to come.
- Corporate COVID-19 strategy leaders need to have a vision of what to expect in the coming months, and a framework for putting into context the news of the day – good and bad.
- A recent report by McKinsey titled When will the COVID-19 pandemic end? does an excellent job presenting both realistic expectations and a framework for interpreting new information.
- Of note, the report describes a “transition to normalcy” – a period of time we’ll begin to experience by spring that will be enabled by the vaccination of vulnerable and exposed populations. With much-lower rates of severe illness, hospitalization and death, there will be a desire and ability to take steps toward normal work and social lives.
- Advocating for the priority vaccination of vulnerable and exposed populations and having a plan to navigate the transition to normalcy is among the implications for businesses to account for in their COVID-19 strategies.
Here, There, and In-Between: Preparing for the “Transition to Normalcy”
I had wondered what would feed our news cycles after the inauguration, and it has become clear that at least some of the media click bait that will be used to capture our attention in the coming months will consist of breathless headlines about COVID-19. Some of the headlines inspire hope, such as those focused on vaccine approvals. Most, however, will be written to play on fear and doubt. These are headlines about new variants of the COVID-19 virus, the hesitancy among some to be vaccinated, manufacturing or logistical problems, and concerns about vaccine efficacy. For example, recent headlines about efficacy would lead a casual reader to believe that vaccines don’t work, because people are getting sick with COVID-19 despite being vaccinated. Only paragraphs deeper in these stories do we learn that most of those who’ve fallen ill were likely infected before or shortly after their first shot, before it could offer any protection.
The point is that information about COVID-19, vaccines and vaccinations is going to make it seem like the future is more uncertain and more bleak than it is likely to be. Yes, there are questions and concerns and real threats to our progress, but these are balanced by positive developments. If you’re leading your company’s COVID-19 strategy, you can’t afford to be distracted by click-bait-driven concerns. You need to remain well-informed and focused.
Ah…A Balanced Perspective
With all the above as context, it was a breath of fresh air to read When will the COVID-19 pandemic end?, a report that landed in my inbox last week from the bright folks at McKinsey. The report presents a sober assessment of forces and factors that will influence how and when the pandemic will end. In so doing, they provide a sort of framework for making sense of news – good and bad – so we can guide our organizations through this next phase of the COVID-19 journey.
Below I summarize highlights of the report, and then identify five implications for businesses. I recommend reading the McKinsey article in full and sharing it along with the implications below with your colleagues and leadership team. It will help to frame your future conversations and strategy decisions.
Report Highlights
- Herd immunity is likely coming but will probably be delayed to Q4 ’21 or later. A key reason for the delay is that more infectious strains are now circulating, and the more infectious the disease, the higher the proportion of the population that needs to be vaccinated in order to achieve herd immunity. And the higher the vaccination target, the more vaccines need to be manufactured, transported, and delivered into arms of people willing to be vaccinated.
It is that last point the poses the biggest challenge. While the proportion of people who say they are likely to be vaccinated has been rising, it currently tops out around 70%, and it looks like we’re going to need 80% or more of the total population to be vaccinated to achieve herd immunity.
- Before we reach herd immunity, we will experience a “transition to normalcy. This is said so well in the article: “A transition toward normalcy will occur when COVID-19 mortality falls, and the disease is de-exceptionalized in society. COVID-19 will not disappear during this transition but will become a more normal part of the baseline disease burden in society (like flu, for example), rather than a special threat requiring exceptional societal response.” During this time, public health measures will still be required, but because the threat of severe illness and death is greatly reduced, social and economic activity will become more normalized.
This in-between time will be tricky to navigate. We won’t be completely safe from COVID-19, but our most vulnerable will be largely protected. Decisions will need to be made about whether, when and how to relax certain prevention measures.
- A balance of forces and factors to watch. Yes, variants are emerging, but this is not unexpected, and it appears vaccines are offering protection against new strains. Yes, there have been problems with distribution, but problems are being solved and collaborators (including private companies) are jumping in to improve systems and efficiencies. Yes, vaccines from Pfizer and Moderna are not enough to cover the US population, but prospects are good for vaccines from AstraZeneca, J&J and Novavax, and if all goes well, we’ll have more than enough. Yes, some people are hesitant to be vaccinated, but with the exception of a relatively small group of committed vaccine opponents, the trend is toward adoption.
Implications for Employers
- Advocate for the vaccination of vulnerable populations. We’re seeing pockets of impatience for phased roll-out plans that prioritize vulnerable and exposed populations. This is self-defeating, because until the most vulnerable and most exposed among us are protected, we cannot begin the transition to normalcy. Certainly we’ve seen some disregard the safety of others from the beginning, but a majority of people want to know that the vulnerable and exposed people they know are protected before they will feel comfortable with any sort of return toward normalcy.
- Focus on vaccinating your workforce (and beyond). Recent articles have focused on strategies to achieve corporate and public vaccination targets and on communication tips to drive vaccination. In both articles, I provide recommendations to make workforce vaccinations more effective and advocate for leveraging your vaccination strategy and infrastructure to offer vaccines to family members, suppliers, customers, and the community at large. The faster your families, supply chain partners and communities in which you operate achieve vaccination targets, the more quickly everyone can begin to live and work in ways that are more normal.
- Site- and community-specific strategies are needed. Different communities are going to achieve vaccination goals at different times, and communities will respond differently when vulnerable populations are vaccinated. For instance, based on what we’ve seen so far people in rural communities are likely to push toward normalization of work and social behaviors more quickly and aggressively than in urban environments. Site-based strategies should be tailored to their local circumstance, striving as always to keep workers safe while enabling business operations to the extent possible.
- Plan to tie any easing of prevention measures to the achievement of vaccination targets. For maximum safety, prevention measures (e.g., distancing, masking, sanitizing) should be kept fully in place until herd immunity is achieved. Realistically, that’s going to be very difficult to enforce and will begin to seem increasingly nonsensical to your employees. It is better to plan for the loosening of some prevention measures, and to tie changes to the achievement of vaccination milestones. This will align incentives to encourage vaccination participation.
So what does this look like? Perhaps masks will no longer be required in a manufacturing plant once 85% of employees are vaccinated. Until herd immunity (at least among your employees) is achieved, it will be a bad idea for employees to crowd into a conference room, but perhaps some rules around office space density, distancing and mask-wearing can be eased once 70% of people are vaccinated.
The above are not recommendations, but examples to stimulate thinking and planning for the in-between period when we’re not fully safe, but risks have been significantly reduced. Specific recommendations will need to consider specific circumstances.
- Support public health. The McKinsey article identifies some plausible scenarios in which COVID-19 remains a threat for the foreseeable future. This pandemic has demonstrated the human and economic consequences of under-staffed and under-resourced public health systems. In politics, memories are short. Businesses should press their legislators for specific plans to strengthen state and county public health departments so that we can be better prepared to manage a possible long tail of COVID-19 threat or respond to new threats that will emerge in the future.
It is clear that the media environment is going to feed the public (including your company’s executives) a steady diet of attention-grabbing headlines and inaccurate and incomplete stories about COVID-19, vaccines, and vaccinations. The coming period will be yet another test for those leading COVID-19 strategies for their companies. Knowing what to expect and having a framework to evaluate new information can help leaders remain focused while interpreting and responding appropriately to new opportunities and threats.
Certainly, my team and I have endeavored to be a source of solid information and actionable insight throughout this pandemic. If there are topics you want us to address, or if you have feedback to share, please let us know.
Ben Hoffman, MD, MPH
Chief Medical Officer, WorkSTEPS
Dr. Hoffman was recently featured on an episode of Workplace Injury Prevention – A Fit For Work Podcast, covering topics including the science behind vaccines, developing herd immunity, mitigation measures for the workplace, and the importance of perseverance as the light at the end of this pandemic’s tunnel grows brighter. Click this link to listen to the episode.
For more from Dr. Hoffman, connect with him on LinkedIn.
Medical:
Global:
UK reports B117 variant could be deadlier: In a major development last Friday, health officials in the UK warned the more transmissible B117 variant, first detected in December, may be also be more deadly. UK’s Prime Minister announced there is some evidence that the B117 variant is associated with higher mortality. The new findings come from a study Friday from by the UK’s New and Emergency Respiratory Advisory Group (NERVTAG), which said a preliminary analysis shows that increased severity may be associated with the variant. NERVTAG is collecting more data to increase the sample size and the trends will become clearer over coming weeks.
Denmark is sequencing all coronavirus samples: Cases involving the variant are increasing 70 percent a week in Denmark, despite a strict lockdown, according to Denmark’s State Serum Institute, a government agency that tracks diseases and advises on health policy. The institute announced this past week that the nation has begun sequencing every positive coronavirus test to check for mutations. The country has sharply increased its sequencing capacity and aims to analyze the genetic virus material in all positive tests. More than 33% of positive tests in the second week of this year have been sequenced so far.
National:
The devastating fall and winter wave of coronavirus infections across the U.S. appears to have finally peaked. While another surge remains possible, especially with new, more infectious variants, the number of new daily infections in the current wave appears to have hit a high in the past week or two and has been declining in most states since.
Moderna retains neutralizing activity against variants: On Monday, Moderna announced that their vaccine is fully protective against the UK B117, but observed a 6-fold reduction in neutralizing titers with South African variant B1351. Despite this, neutralizing titer levels with B1351 remain above levels expected to be protective. Nonetheless, Moderna stated on Monday that its clinical strategy is to proactively address the pandemic as the virus continues to evolve. First, the company will test an additional booster dose of its current COVID-19 Vaccine (mRNA-1273) to study the ability to further increase neutralizing titers and will also advance a Phase 1 clinical trial of MRNA-1273.351 an emerging variant booster.
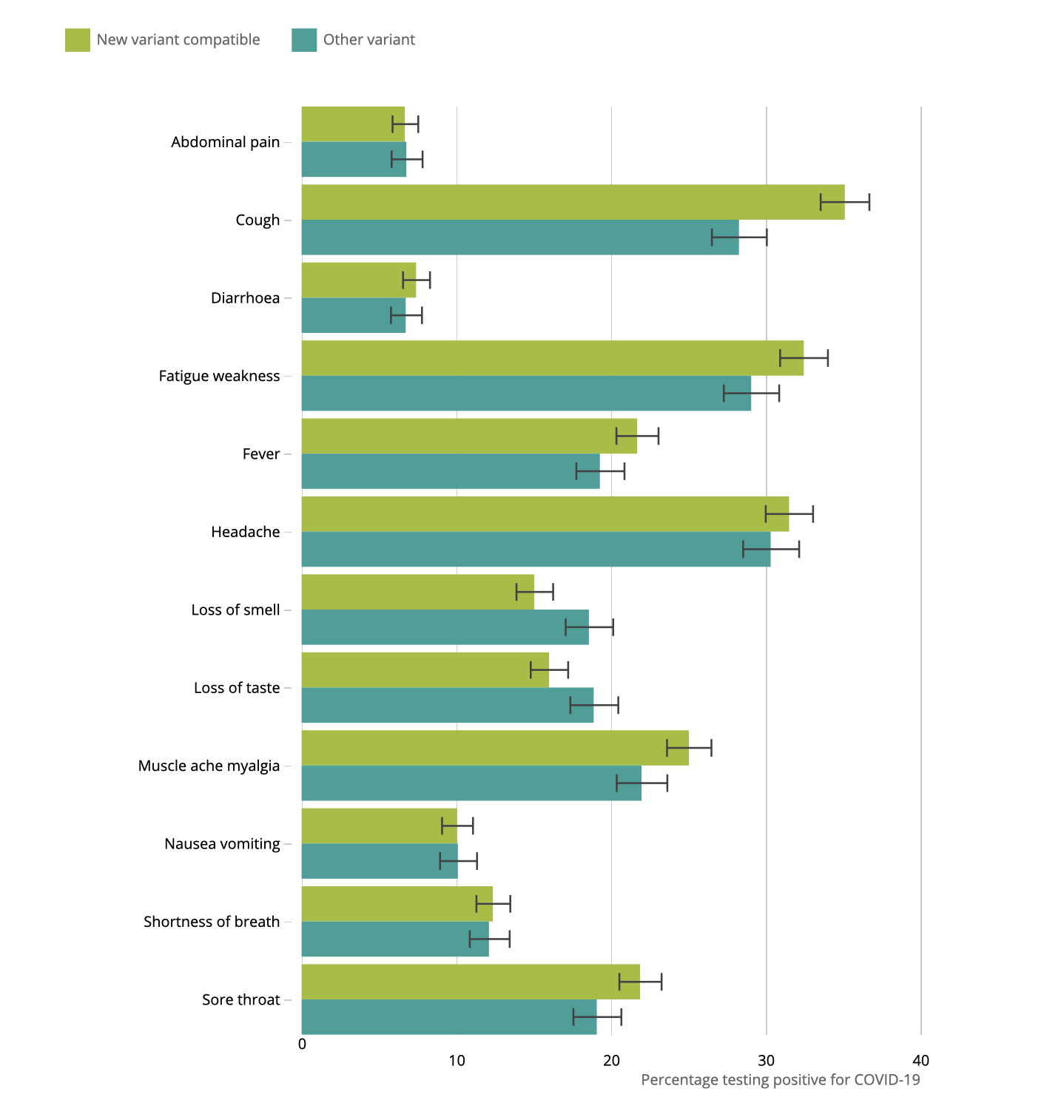
Variant B117 – UK National Symptoms Survey Results: According to a UK Govt. prevalence survey, symptoms of the ‘new’ B.1.1.7 COVID-19 variant don’t seem massively different from the ‘old’ variant. Cough, sore throat, fatigue & muscle ache are a somewhat more common. Regarding transmission, the increase in coughing does seem notable (35% new, 28% old) – especially if more virus is shed in the upper respiratory tract. Other symptoms: fatigue/weakness (33% new, 29% old); headache (32% new, 30% old); muscle ache (25% new, 22% old); sore throat (22% new, 19% old); fever (22% new, 19% old); loss of smell (15% new, 19% old); loss of taste (16% new, 19% old); breathlessness (12% both); nausea/vomiting (10% both); diarrhea (7% both); abdominal pain (7% both).
Long-term smoking highly associated with COVID-19 severity: According to a study published on Wednesday, people who have smoked for more than 30 pack-years—a unit for cumulative smoking—are about twice as likely to be hospitalized and to die after testing positive for COVID-19 as nonsmokers. The researchers reviewed records from 7,102 patients who were in Cleveland Clinic’s COVID-19 registry from Mar 8 through Aug 25, 2020. Scientists found that people who had smoked for more than 30 pack-years were 2.25 times more likely to be hospitalized after a positive COVID-19 test and 1.89 times more likely to die following diagnosis compared with nonsmokers (95% CI, 1.29 to 1.76). The association is likely mediated in part by comorbidities.
Mitigation / Suppression:
Change in Reported Adherence during pandemic: According to a research survey data published by Johns Hopkins scientists this week, self-reported adherence to COVID-19 mitigation behaviors such as physical distancing fell substantially—while mask wearing rose significantly—from spring to fall 2020, regardless of US Census region. The researchers asked all participants to complete a survey every 14 days on 16 evidence-based nonpharmaceutical interventions (NPIs). Among the 7,705 participants who completed all survey waves, the NPI index showed peak compliance at the beginning of the pandemic (70.0 in early April), a leveling off in June (high 50s), and a slight climb to 60.1—but still much lower than in the spring—at the end of the survey in November.
Data from health departments on case investigation and contact tracing: Last week, an analysis published by the CDC of case investigation data from 56 US health departments showed that heavy investigator caseloads and an unengaged public hampered the ability to locate and quarantine contacts in a timely manner. The study used health department reports from Jun 25 to Jul 24, 2020. Researchers reported an inverse relationship between investigator caseload and timely interviewing of patients and number of contacts per case. The median caseload per investigator was 31 (range, 1 to 196), and the median number of contacts assigned for follow-up per investigator was 29 (range, 0.5 to 200). When contact tracers had heavier caseloads, the percentage of coronavirus patients interviewed within 24 hours of case report fell, as did the number of contacts identified per patient.
Double Masking: This week, US public health expert Dr. Fauci noted in an interview that he was in favor of wearing two masks. He stated that if you have a physical covering with one layer, you put another layer on, it likely would be more effective. In places where it’s difficult to maintain social distance, such as on an airplane or at the store, two masks would provide additional protection. He added that using two masks creates an obstacle course for the viral particle to make its way from the air into your nose and throat and then into your lungs. Several public officials were photographed wearing two masks during the inauguration last week.
Corporate:
High antibodies noted in public service workers: A study published Tuesday showed that, while only 10.1% of first responders and public service personnel in New York City reported positive COVID test results, 22.5% had COVID-19–specific antibodies in their blood, with higher rates in prison staff and emergency transport staff (EMTs).The study ran from May 18 – Jul 2, 2020, and included 22,647 participants from correctional facilities, emergency medical services, childcares, fire and police departments, and the medical examiner’s office. The researchers found that correctional staff and EMTs had the highest rates of seroprevalence at 39.2% and 38.3%, respectively. Workers who wore PPE all the time also had higher seropositivity rates; researchers suggested this could be due to higher exposure risks on the job, improper PPE use, insufficient training, or shortage of supplies. These essential workers would be a critical population for vaccine priority.
New travel restrictions into the U.S: From Tuesday 1/25/2021, the CDC will start to require all travelers flying to the US provide proof of a negative COVID-19 test taken within 3 days of their flight. Airlines have been notified by the CDC to deny boarding to any traveler who does not present a test result, or documentation of recovery. The CDC order applies to all travelers 2 years and older and also requires a 7-day period of quarantine for all travelers, regardless of negative test status. This week, the US also enacted strict travel bans to limit foreign travelers who may be infected with variant strains of COVID-19. The ban extends to all non-US citizens traveling to America from the UK, Ireland, and 26 countries in Europe, Brazil and South Africa. Of concern are the UK, and South African variants. Masks will also be required on passengers age 2 and older on all airplanes, ferries, trains, subways, buses, taxis, and ride-share vehicles in the United States.
Vaccine considerations: As more people get vaccinated, we anticipate questions from employees who have been vaccinated regarding continuation of mitigation practices. Per CDC, experts need to understand more about the protection that COVID-19 vaccines provide in real-world conditions before making that decision. Other factors, including how many people get vaccinated and how the virus is spreading in communities. Vaccination protects the recipient from severe disease and potential fatality. CDC states not much is known yet whether getting a COVID-19 vaccine will prevent the recipient from spreading the virus that causes COVID-19 to other people, even if the recipient themselves don’t get sick. While more data about the protection that COVID-19 vaccines provide under real-life conditions, it will be important for everyone to continue using all the tools available to help stop this pandemic.

Chief Medical Officer

Medical Director

Director of Case Management

Nurse Case Manager

Nurse Case Manager

Nurse Case Manager

Strategic Communications Consultant
This Guidance (“Guidance”) is provided for informational and educational purposes only. It is not intended as Legal Advice or Medical Advice. Adherence to any recommendations included in this Guidance will not ensure successful diagnosis or treatment in every situation. Furthermore, the recommendations contained in this Guidance should not be interpreted as setting a standard of care or be deemed inclusive of all proper methods of care nor exclusive of other methods of care reasonably directed to obtaining the same results. The ultimate judgment regarding the propriety of any specific therapy must be made by the physician and the patient in light of all the circumstances presented by the individual patient, and the known variability and biological behavior of the medical condition. Similarly, this Guidance is based on current advice, comments, and guidance from the EEOC, CDC and the CMS made publicly available. The ultimate judgement regarding the propriety of any specific employment action must be made by the company and attorney in light of all of the circumstances presented by the company, state and federal rules existing at the time and the then current state of the National Pandemic. This Guidance and its conclusions and recommendations reflect the best available information at the time the Guidance was prepared. The results of future studies or changes in rules, regulations or laws may require revisions to the recommendations in this Guidance to reflect new data. WorkSTEPS does not warrant the accuracy or completeness of the Guidance and assumes no responsibility for any injury or damage to persons or property arising out of or related to any use of this Guidance or for any errors or omissions.